
Flatfoot (in medicine Pes planus) is a condition in which the medial longitudinal arch of the foot is diminished or absent. Around 30% of adults have pes planus, however the majority does not have any symptoms. Flatfoot may be congenital or acquired.
Congenital:
- Rigid: due to structural bony abnormalities (tarsal coalition, vertical talus)leading to poor shock absorption.
- Flexibile (often hereditary and common in children), it leads to stress of muscle, ligaments. Speed is lost due to no rigid lever for propulsion
Acquired leading to a diverse range of deformity and symptoms.
Causes
- Adults
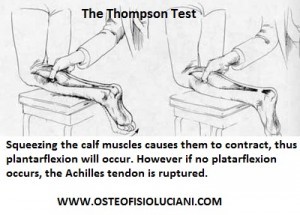
- acquired: dysfunction of the tibialis posterior tendon (most common), tear of the spring ligament, rupture of the tibialis anterior (both rare).
- physiological: lack of normal arch development (possibly due to ligamentous laxity).
- degenerative changes:osteoarthritis, inflammatory arthropathy, fractures.
- neuropathic: diabetes, polio, etc.
- Children
- physiological: infants often have minimal arch, while many toddlers have flattening of the long arch, with forefoot pronation and heel valgus on weight-bearing. However by the age of 10 most of the children spontaneously develop a strong normal arch.
- abnormal development of the foot may be due to: neurological problems (such as polio, cerebral palsy) or bony (fusion of two or more tarsals “tarsal coalition”), ligamentous abnormalities.
There are many contributing factors such us:
- Footwear: shoes which limit toe movement; high heels.
- A tight Achilles tendon or calf muscles (heel cord contracture).
- Obesity
- Ligamentous laxity (Marfan’s syndrome, pregnancy, etc).
- Repetitive microtrauma (higher mileage in running)
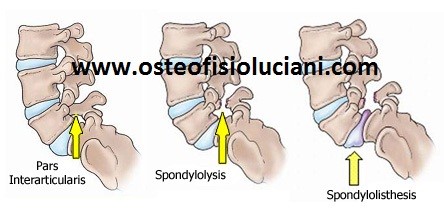
- Bony abnormalities, eg rotational deformities, tibial abnormalities, coalition (fusion) of tarsal bones, equinus deformity.
- Other factors causing foot pronation, eg hip abductor weakness and genu valgum
Diagnosis
- Observe the flatfoot: With the patient standing, look at his or her feet from above and behind. Loss of the arch is visible, with the medial side of the foot close to the ground. Look at the feet from behind – with Pes Planus the heel bone is everted or in valgus (outwards). The forefoot is abducted relative to the hindfoot. More than 2 toes can be seen outside the heel.
- Is the flatfoot flexible?: Ask the patient to stand on tiptoe. With flexible flatfoot, this will reveal the arch, and the heel will move inwards (varus position).
- Look for signs of tibialis posterior dysfunction[(if history is suggestive of this).
- Ask the patient: to do 10 unsupported heel raises (stand on one foot on tiptoe, unsupported). Patients with tibialis posterior dysfunction will be unable to do this
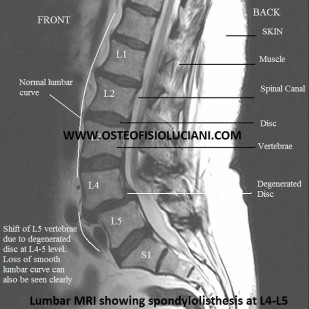
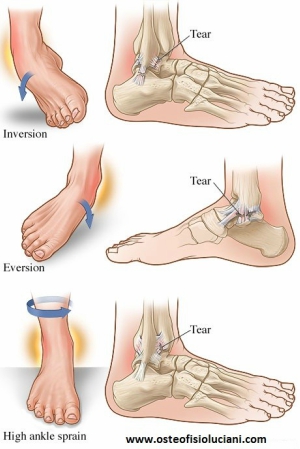
Flatfoot (Pes planus) may present as a symptomatic (causing pain in the foot) or asymptomatic (causing no pain) findings on examination. Therefore may cause or be associated with other bio-mechanical causes of pain such as:low back pain, genus valgum (knock knees), medial or anterior knee pain, shin splints, achilles tendinopathy, increased risk of ankle sprain, plantar fasciitis. This is due to poor shock absorption by ligaments and muscle of the foot, thereby all the impacts are transmitted to the joints above-ankle, knees, hips, low back,neck, etc. Fibrous contracture of the peronei muscles may be noted.
Do not forget to look at the patient has a whole as flatfeet may cause headaches!!! Remember to consider other areas (see picture below) and…

…to look at the shoes.
Runners and flat foot.
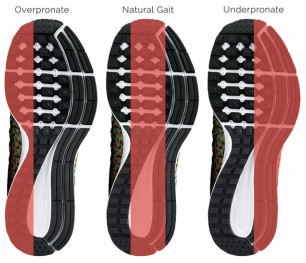
It is generally accepted by professionals that a person with flat feet tends to overpronate in his or her running form. However, persons with flat feet may also have a neutral or underpronating gait. Pronation is a natural form of shock absorption during running and walking, when the ankle rolls inward and the weight distribution in the foot shifts medially. Overpronation is excessive pronation; it disrupts the alignment of the leg and may result in injuries due to over-stressing of the knee and leg. With normal, or neutral, running shoes, a person who overpronates in his or her running form may be more susceptible to shin splints, back problems, and tendonitis in the knee. Running in shoes with extra medial support or using special shoe inserts, orthoses, may help correct one’s running form by reducing pronation and may reduce risk of injury.
Very good link explaining normal pronation,under pronation and over pronation in running.
Treatment.
Treatment can be either non-surgical or surgical.
- Non-surgical treatment:
- Othotics (orthotic devices such as arch supports and custom-made orthoses).
- Muscle rehabilitation
- Manipulation
- Dry needling
- Soft tissue
- Stretching exercise
- Taping
- Surgical
- Arthrodesis, or welding (fusing) one or more of the bones in the foot/ankle together
- Osteotomy, or cutting and reshaping a bone to correct alignment
- Excision, or removing a bone or bone spur
- Synovectomy, or cleaning the sheath covering a tendon
- Tendon transfer, or using a piece of one tendon to lengthen or replace another
Complications
Hallux Valgus (because more weight is borne by the medial metatarsals when the foot hyperpronates). Plantar fascitis. Metatarsalgia. Tibialis posterior dysfunction (because hyperpronation stretches this tendon). Knee pain. Low back pain/SIJ pain as flatfoot may reduce the shock-absorbing features of the foot.
Hints
- Flatfoot may be due to other causes such as Charcot and posterior tibialis dysfunction, see a physiotherapist, osteopath, chiropractor for further information or advices.
- Wear shoes with low heels and wide toes.
- Lose weight if appropriate.
- In cases of severe flat feet, orthoses should be used through a gradual process to lessen discomfort .
- Arch supports used without correcting heel cord contracture can make symptoms worse.
Heel cord stretching is an important part of treatment, as a tight Achilles tendon tends to pronate the foot.
Dott. Emanuele Luciani
Osteopath, physiotherapist, hatha yoga teacher
Osteopath registered with the General Osteopathic Council (GOsC)
(number 8232http://www.osteopathy.org.uk/home/)
"Centro Studi Tre Fontane"
Via Luigi Perna 51, Rome


















 Surgery
Surgery




